The most common causes of lumbar pain are spinal diseases, especially degenerative-dystrophic (osteochondrosis, spondylosis deformity), and back muscle tension. In addition, various diseases of the abdominal cavity and small pelvis, including tumors, can cause symptoms similar to a herniated disc, pressing on the roots of the spine.
It is no coincidence that such patients only turn to neurologists, but also to gynecologists, orthopedists, urologists, and most importantly, of course to district or family doctors.
Etiology and pathogenesis of lumbar pain
According to modern concepts, the most common causes of lumbar pain are:
- pathological changes in the spine, especially degenerative-dystrophic;
- pathological changes in muscles, often myofascial syndrome;
- pathological changes in the abdominal organs;
- diseases of the nervous system.
Risk factors for lumbar pain are:
- strenuous physical activity;
- uncomfortable working posture;
- injuries;
- cooling, draft;
- alcohol abuse;
- depression and stress;
- occupational diseases associated with high temperature exposure (in particular, in hot shops), radiation energy, with sharp temperature fluctuations, vibrations.
Among the causes of lumbar vertebral pain are:
- root ischemia (discogenic radicular syndrome, discogenic radiculopathy), caused by root compression by a herniated disc;
- reflex muscle syndrome, which can be caused by degenerative-dystrophic changes in the spine.
A particular role in the occurrence of back pain can be played by various functional disorders of the lumbar spine, when intervertebral joint block appears due to incorrect posture and impaired mobility. At joints located above and below the block, compensatory hypermobility develops, leading to muscle spasm.
Signs of acute spinal canal compression
- numbness in the perineal area, weakness and numbness of the legs;
- delayed urination and defecation;
- with spinal cord compression, a decrease in pain is observed, alternating with numbness in the pelvis and pelvic limbs.
Lumbar pain in childhood and adolescence is most often caused by anomalies in spinal development. Non -growth of the vertebral arch (spina bifida) occurs in 20% of adults. Examination showed hyperpigmentation, birthmarks, multiple scars, and skin hyperkeratosis in the lumbar region. Occasionally there is urinary incontinence, trophic disorders, weakness in the legs.
Lumbar pain can be caused by lumbari - the transition of the S1 vertebra in relation to the lumbar spine - and sacralization - the connection of the L5 vertebra to the sacrum. This anomaly is formed due to the individual characteristics of the development of transverse processes of the vertebrae.
Nosological forms
Almost all patients complain of back pain. The disease is manifested mainly by inflammation of inactive joints (intervertebral, costo-vertebral, lumbosacral joints) and spinal ligaments. Gradually, oscillations develop in it, the spine loses its elasticity and functional mobility, becoming like a bamboo stick, brittle, easily injured. At the stage of obvious clinical manifestations of the disease, chest movements during breathing and, as a consequence, the vital capacity of the lungs decreases significantly, which contributes to the development of a number of pulmonological diseases.
Spinal tumors
Distinguish between benign and malignant tumors, mainly of spinal and metastatic origin. Benign spinal tumors (osteochondroma, chondroma, hemangioma) are sometimes clinically asymptomatic. With hemangiomas, spinal fractures can occur even with minor external influences (pathological pathology).
Malignant tumors, especially metastatic, originate in the prostate gland, uterus, breasts, lungs, adrenal glands and other organs. The pain in this case is much more frequent than in benign tumors - usually persistent, painful, exacerbated by slight movements, making the patient not rest and sleep. Characterized by progressive deterioration of the condition, increased general fatigue, significant changes in the blood. Very important for diagnosis are radiography, computed tomography, magnetic resonance imaging.
Osteoporosis
The main cause of this disease is a decrease in the function of the endocrine glands due to independent disease or against the background of general aging of the body. Osteoporosis can develop in patients who take hormones for a long time, chlorpromazine, anti-tuberculosis drugs, tetracycline. Radicular disorders that accompany back pain arise as a result of deformation of the intervertebral foramen, and the spine (myelopathy) - caused by compression of the radiculomedullary arteries or fractures of the spine, even after minor injuries.
Myofascial syndrome
Myofascial syndrome is a leading cause of back pain. It can occur as a result of too much energy (during strenuous physical exercise), excessive bruising and muscle bruising, non -physiological posture while working, reactions to emotional stress, shortening of one leg, and even flat feet.
Myofascial syndrome is characterized by the presence of a "trigger" zone (trigger point), a pressure that causes pain, often radiating to neighboring areas. In addition to myofascial pain syndrome, inflammatory muscle disease - myositis can also cause pain.
Lumbar pain often occurs with diseases of internal organs: gastric ulcer and duodenal ulcer, pancreatitis, cholecystitis, urolithiasis, and others. They can be pronounced and mimic the picture of lumbago or discogenic lumbosacral radiculitis. However, there are also clear differences, which make it possible to distinguish the reflected pain from the disease arising from the disease of the peripheral nervous system, which is caused by the symptoms of the underlying disease.
Clinical symptoms for lumbar pain
Most often, low back pain occurs at the age of 25–44 years. Distinguish between acute, prolonged pain, as a rule, 2-3 weeks, and sometimes up to 2 months. , And chronic - more than 2 months.
Compression radicular syndrome (discogenic radiculopathy) is characterized by a sudden onset, often after weight lifting, sudden movements, hypothermia. Symptoms depend on the location of the lesion. At the heart of the syndrome is root compression by a herniated disc, which occurs as a result of dystrophic processes, facilitated by static and dynamic loads, hormonal disorders, trauma (including spinal microtraumatics). Often, the pathological process involves the root area of the spine from the dura mater to the intervertebral foramen. In addition to disc herniation, bone growth, cicatricial changes in epidural tissue, and hypertrophied ligamentum flavum can be involved in trauma to the roots.
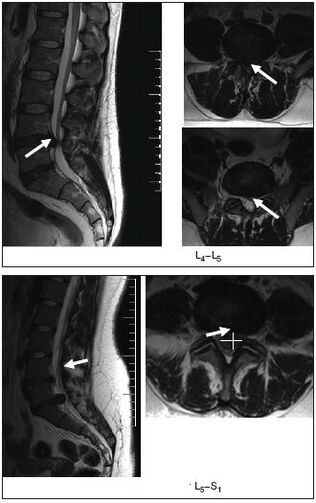
Upper lumbar roots (L1, L2, L3) rarely suffer: they do not exceed 3% of all lumbar radicular syndromes. Twice more often, the L4 root was affected (6%), resulting in a characteristic clinical picture: mild pain along the lower and frontal surface of the thigh, the middle surface of the lower leg, paresthesia (numbness, burning, crawling) in this area; slight weakness of the quadriceps. The knee reflex is constant, and sometimes even increased. The L5 root was most frequently affected (46%). The pain is localized in the lumbar and gluteal regions, along the outer surface of the thigh, the antero-outer surface of the lower leg to the feet and fingers III – V. It is often accompanied by a decrease in the sensitivity of the anterior skin - the outer surface of the foot and strength on the extensor of the fingers III - V. It is difficult for the patient to stand on the heel. With long -term radiculopathy, hypotrophy of the anterior tibialis muscle develops, and the S1 root is often affected (45%). In this case, the pain in the lower back radiates along the outer surface of the thigh, the outer surface of the leg and the lower leg. Examination often shows hypalgesia of the posterior-external foot surface, decreased triceps muscle strength and flexion of the toes. It is difficult for such patients to stand on their toes. There is a decrease or loss of the Achilles reflex.
Vertebral lumbar reflex syndrome
It can be acute and chronic. Acute lower back pain (LBP) (lumbago, "lumbago") occurs within minutes or hours, often suddenly due to awkward movements. The stabbing, shooting pain (like electric shock) is localized to the entire lower back, sometimes radiating to the iliac and buttocks area, increases sharply with coughing, sneezing, decreases in the supine position, especially if the patient finds a comfortable position. Movement in the lumbar spine is limited, lumbar muscles tense, Lasegue symptoms caused, often bilateral. Therefore, the patient lies on his back with his legs extended. The doctor simultaneously flexes the affected leg at the knee and hip joints. This does not cause pain, because at this position of the foot, the aching nerve is loosened. Then the doctor, letting the leg be bent at the hip-hip joint, begins to bend it at the knee, thus causing tension in the sciatic nerve, which gives a strong pain. Acute lumbodynia usually lasts 5-6 days, sometimes less. The first attack ends faster than the next attack. Recurrent lumbago attacks tend to develop into chronic PB.
Abnormal back pain
A number of differentiated clinical symptoms are not uncommon for back pain caused by degenerative-dystrophic changes in the spine or myofascial syndrome. These signs include:
- the appearance of pain in childhood and adolescence;
- back injury immediately before the onset of lower back pain;
- back pain accompanied by fever, or signs of intoxication;
- backbone;
- rectum, vagina, both legs, belt pain;
- lower back pain contact with eating, defecation, intercourse, urination;
- necological pathology (amenorrhea, menstruation, vaginal discharge), which appears against the background of back pain;
- increased pain in the lower back in a horizontal position and a decrease in vertical position (Razdolsky symptoms, characteristic of tumor processes in the spine);
- persistent increase in pain for one to two weeks;
- limbs and the appearance of pathological reflexes.
Survey method
- external examination and palpation of the lumbar region, detection of scoliosis, muscle tension, pain and trigger points;
- determination of range of motion in the lumbar spine, areas of muscle wasting;
- neurological status research; determination of tension symptoms (Lassegh, Wasserman, Neri). [Study on Wasserman symptoms: knee flexion in patients in a cartilage condition causes pain in the hip. Neri symptom study: sharp bending of the head to the chest of a patient lying on his back with legs straight, causing acute pain in the lower back and along the sciatic nerve.
- study of state of sensitivity, reflex spheres, muscle tone, autonomic disturbances (swelling, discoloration, temperature and moisture of the skin);
- radiography, magnetic resonance imaging of the spine.
MRI is very informative.
- ultrasound examination of the pelvic organs;
- gynecological examination;
- if necessary, additional studies are performed: cerebrospinal fluid, blood and urine, sigmoidoscopy, colonoscopy, gastroscopy, etc.
Treatment
Acute lower back pain or exacerbation of vertebral or myofascial syndrome
Undifferentiated treatment. Soft motor mode. With severe pain in the first few days, rest in bed, and then walk on crutches to relieve the spine. The bed should be sturdy, wooden boards should be placed under the mattress. For warming, a wool scarf, electric heating pad, sandbag or heated salt are recommended. Ointments have a good effect: finalgon, tiger, capsin, diclofenac, etc. , as well as mustard plaster, pepper plaster. Ultraviolet irradiation is recommended in erythema doses, leeches (taking into account possible contraindications), irrigation of painful areas with ethyl chloride.
Anesthetic effects are provided by electrical procedures: percutaneous electroanalgesia, sinusoidal modulation currents, diadynamic currents, electrophoresis with novocaine, and others. The use of reflexology (acupuncture, laser therapy, moxibusi) is effective; novocaine blockade, trigger point pressure sequence.
Drug therapy includes analgesics, NSAIDs; sedatives and / or antidepressants; drugs that reduce muscle tension (muscle relaxation). In case of arterial hypotension, tizanidine should be prescribed with caution because of its hypotensive effects. If swelling of the spinal roots is suspected, a diuretic is prescribed.
The main analgesics are NSAIDs, which are often used uncontrollably by patients when pain increases or recurs. It should be noted that long -term use of NSAIDs and analgesics increases the risk of complications of this type of therapy. Currently, there are many NSAID options. For patients suffering from pain in the spine, in terms of availability, efficacy and less likelihood of side effects (gastrointestinal bleeding, dyspepsia), diclofenac 100–150 mg / day is preferred over "non-selective" medications. in, intramuscularly, rectal, topically, ibuprofen and ketoprofen in 200 mg and topically, and from "selectively" - meloxicam in 7. 5-15 mg / day, nimesulide in 200 mg / day.
In NSAID treatment, side effects may occur: nausea, vomiting, loss of appetite, pain in the epigastric region. Possible ulcerogenic action. In some cases, there may be ulceration and bleeding in the gastrointestinal tract. In addition, headache, dizziness, drowsiness, allergic reactions (skin rash, etc. ) were observed. Treatment is contraindicated in ulcerative processes in the gastrointestinal tract, pregnancy and lactation. To prevent and reduce dyspeptic symptoms, it is recommended to take NSAIDs during or after eating and drinking milk. In addition, NSAID intake with increased pain along with other medications patients take to treat comorbidities, results, as observed with long -term treatment for many chronic diseases, to decreased adherence to treatment and, as a consequence, inadequate therapeutic efficacy.
Thus, modern conservative treatment methods include the use of mandatory drugs that have chondroprotective, chondrostimulating effects and have a better therapeutic effect than NSAIDs. This need is fully met by the drug Teraflex-Advance, which is an alternative to NSAIDs for mild to moderate pain syndromes. One Teraflex-Advance drug capsule contains 250 mg of glucosamine sulfate, 200 mg of chondroitin sulfate and 100 mg of ibuprofen. Chondroitin sulfate and glucosamine are involved in connective tissue biosynthesis, help prevent cartilage destruction, stimulate tissue regeneration. Ibuprofen has analgesic, anti-inflammatory, antipyretic effects. The mechanism of action is due to selective inhibitors of cyclooxygenase (COX type 1 and type 2) - the main enzyme of arachidonic acid metabolism, which causes a decrease in prostaglandin synthesis. The presence of NSAIDs in the preparation of Teraflex-Advance helps to increase the range of motion in the joints and reduces morning stiffness in the joints and spine. It should be noted that, according to R. J. Tallarida et al. , The presence of glucosamine and ibuprofen in Teraflex-Advance provides synergy in relation to the analgesic effect of the latter. In addition, the analgesic effect of the glucosamine / ibuprofen combination was given as much as 2. 4 times the dose of ibuprofen.
After relieving the pain, it is desirable to switch to Teraflex, which contains the active ingredients chondroitin and glucosamine. Teraflex is taken 1 capsule 3 times a day. for the first three weeks and 1 capsule 2 times / day. in the next three weeks.
In most patients, when taking Teraflex, there is a positive tendency in the form of pain syndrome and a decrease in neurological symptoms. The drug is well tolerated by patients, no manifestations of allergies are observed. The use of Teraflex in degenerative-dystrophic diseases of the spine is rational, especially in young patients, both in combination with NSAIDs and as monotherapy. In combination with NSAIDs, the analgesic effect occurs 2 times faster, and the need for doses of NSAID therapy is progressively reduced.
In clinical practice, for lesions of the peripheral nervous system, including those associated with spinal osteochondrosis, B vitamins with neurotropic effects are widely used. Traditionally, the method of replacement of vitamins B1, B6 and B12, 1-2 ml is used. intramuscularly alternately daily. The course of treatment is 2-4 weeks. Disadvantages of this method include the use of small doses of drugs that reduce the effectiveness of treatment and the need for frequent injections.
For discogenic radiculopathy, traction therapy is used: traction (including underwater) in a neurological hospital. In case of myofascial syndrome after local treatment (novocaine blockade, irrigation with ethyl chloride, anesthetic ointment), hot compresses are applied to the muscles for several minutes.
Chronic back pain of vertebrogenic or myogenic origin
If the disc is herniated, it is recommended:
- wearing a weightlifter belt type rigid corset;
- sudden elimination of movement and inclination, limitation of physical activity;
- physiotherapy exercises to create muscular corsets and restore muscle mobility;
- massage;
- novocaine blockade;
- reflexology;
- physiotherapy: ultrasound, laser therapy, heat therapy;
- intramuscular vitamin therapy (B1, B6, B12), multivitamins with mineral supplements;
- for paroxysmal pain, carbamazepine is prescribed.
Non -drug treatment
Although there are effective conservative treatment methods, there are dozens of techniques, some patients require surgical treatment.
Indications for surgical treatment are divided into relative and absolute. The absolute indication for surgical treatment is the development of caudal syndrome, the presence of isolated herniated discs, pronounced radicular pain syndrome, which is not reduced, even if there is continued treatment. The development of radiculomyeloischemia also requires urgent surgical intervention, however, after the first 12-24 hours, the indications for surgery in such cases become relative, first, due to the formation of irreversible changes in the roots, and secondly, because in most cases inIn the process of treatment and recovery, the process will deteriorate in a period of about 6 months. A similar regression period was observed with delayed operation.
Relative indications include the ineffectiveness of conservative treatment, recurrent sciatica. Conservative therapy in duration should not exceed 3 months. and lasts at least 6 weeks. It is assumed that a surgical approach in cases of acute radicular syndrome and ineffectiveness of conservative treatment is allowed in the first 3 months. after the onset of pain to prevent chronic pathological changes in the roots. The relative indication is a case of very pronounced pain syndrome, when the pain component changes with increasing neurological deficits.
From physiotherapeutic procedures, electrophoresis with caripazim proteolytic enzymes are now widely used.
It is known that physical therapy and massage are an important part of the complex treatment of patients with spinal lesions. Therapeutic gymnastics achieves the purpose of strengthening the body in general, increasing efficiency, improving coordination of movements, improving fitness. At the same time, special training aims to restore certain motor functions.




























